| <英語論文>
Effects of a high-prebiotic diet versus probiotic supplements versus synbiotics on adult mental health: The “Gut Feelings” randomised controlled trial
Tanya M Freijy 1 2, Lachlan Cribb 1, Georgina Oliver 1, Najwa-Joelle Metri 3, Rachelle S Opie 4, Felice N Jacka 5 6 7, Jason A Hawrelak 8 9, Julia J Rucklidge 10, Chee H Ng 1, Jerome Sarris 1 2 3
1Professorial Unit, The Melbourne Clinic, Department of Psychiatry, The University of Melbourne, Melbourne, VIC, Australia.
2Faculty of Medicine, Dentistry and Health Sciences, Florey Institute of Neuroscience and Mental Health, University of Melbourne, Melbourne, VIC, Australia.
3NICM Health Research Institute, Western Sydney University, Westmead, NSW, Australia.
4IPAN, School of Exercise and Nutrition Sciences, Deakin University, Melbourne, VIC, Australia.
5School of Medicine, Food and Mood Centre, IMPACT Strategic Research Centre, Deakin University, Melbourne, VIC, Australia.
6Centre for Adolescent Health, Murdoch Children’s Research Institute, Melbourne, VIC, Australia.
7College of Public Health, Medical and Veterinary Sciences, James Cook University, Townsville, OLD, Australia.
8School of Pharmacy and Pharmacology, University of Tasmania, Hobart, TAS, Australia.
9Human Nutrition and Functional Medicine Department, University of Western States, Portland, OR, United States.
10School of Psychology, Speech and Hearing, University of Canterbury, Christchurch, New Zealand.
Abstract
Background:
Preliminary evidence supports the use of dietary interventions and gut microbiota-targeted interventions such as probiotic or prebiotic supplementation for improving mental health. We report on the first randomised controlled trial (RCT) to examine the effects of a high-prebiotic dietary intervention and probiotic supplements on mental health.
Methods:
“Gut Feelings” was an 8-week, 2 × 2 factorial RCT of 119 adults with moderate psychological distress and low prebiotic food intake.
Treatment arms: (1) probiotic supplement and diet-as-usual (probiotic group);
(2) high-prebiotic diet and placebo supplement (prebiotic diet group);
(3) probiotic supplement and high-prebiotic diet (synbiotic group);
and (4) placebo supplement and diet-as-usual (placebo group).
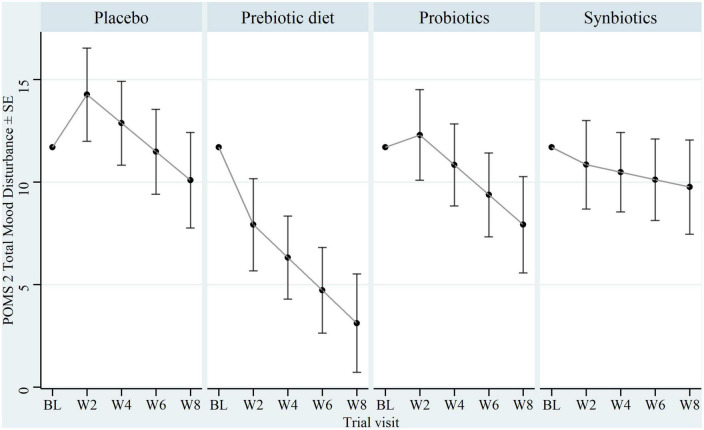
The primary outcome was assessment of total mood disturbance (TMD; Profile of Mood States Short Form) from baseline to 8 weeks. Secondary outcomes included anxiety, depression, stress, sleep, and wellbeing measures.
Results:
A modified intention-to-treat analysis using linear mixed effects models revealed that the prebiotic diet reduced TMD relative to placebo at 8 weeks [Cohen’s d = -0.60, 95% confidence interval (CI) = -1.18, -0.03; p = 0.039]. There was no evidence of symptom improvement from the probiotic (d = -0.19, 95% CI = -0.75, 0.38; p = 0.51) or synbiotic treatments (d = -0.03, 95% CI = -0.59, 0.53; p = 0.92). Improved anxiety, stress, and sleep were noted in response to the prebiotic diet while the probiotic tentatively improved wellbeing, relative to placebo. No benefit was found in response to the synbiotic intervention. All treatments were well tolerated with few adverse events.
Conclusion:
A high-prebiotic dietary intervention may improve mood, anxiety, stress, and sleep in adults with moderate psychological distress and low prebiotic intake. A synbiotic combination of high-prebiotic diet and probiotic supplement does not appear to have a beneficial effect on mental health outcomes, though further evidence is required. Results are limited by the relatively small sample size.
Clinical trial registration:
https://www.anzctr.org.au/Trial/Registration/TrialReview.aspx?id=372753, identifier ACTRN12617000795392.
Keywords: clinical trial; diet; gut microbiota; mental health; mood; prebiotics; probiotics; synbiotics.
Front Neurosci. 2023 Feb 6;16:1097278.
doi: 10.3389/fnins.2022.1097278. eCollection 2022.
PMID: 36815026
PMCID: PMC9940791
DOI: 10.3389/fnins.2022.1097278
|
